Managing and Treating Chronic Constipation
*Please note: This slide show represents a visual interpretation and is not intended to provide, nor substitute as, medical and/or clinical advice.
How is chronic constipation managed and treated?
Chronic constipation (CC) is a long-term bowel problem that affects how your digestive system works. It affects about 15 percent of people in the United States.1
How is chronic constipation managed and treated?
Constipation means either difficulty having a bowel movement or having fewer bowel movements than usual. Some physicians consider you to have constipation when you have fewer than 3 bowel movements a week.1 You might feel like you want to go but cannot, or you might feel like you have not emptied your bowels completely.2,3
This animation tells you about ways to manage and treat chronic constipation.
What is the best way to manage chronic constipation?
The best treatment for chronic constipation depends on how your body responds. Exercising and getting more fiber might work for you, or you might need medication.
Ask your physician if you should keep track of what you eat and drink and of your bowel movements. They can tell you how to do this.
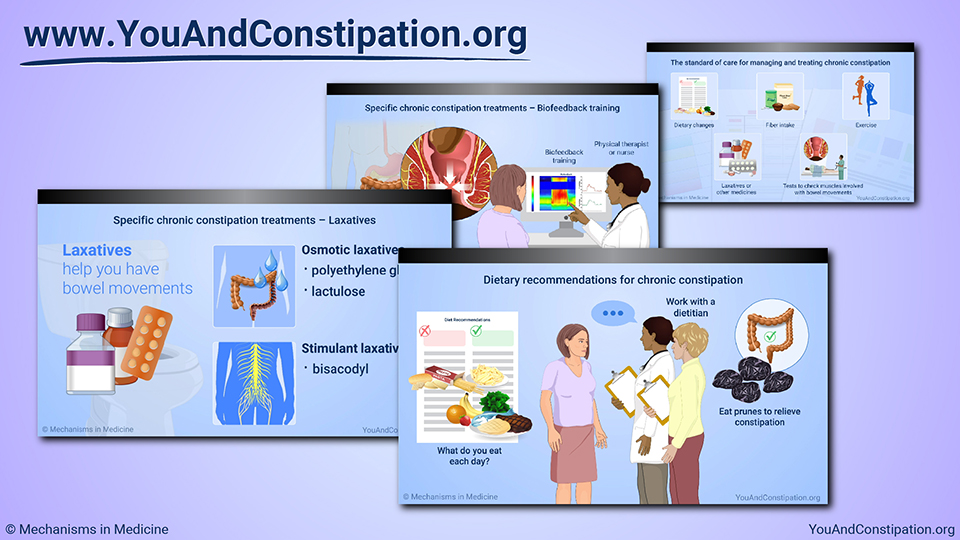
Dietary recommendations for chronic constipation
Your physician will probably recommend diet changes first. They might first ask what you eat each day and recommend changes. They might also ask you to work with a dietitian, a healthcare professional who specializes in diet and nutrition.
Your physician might ask you to eat some dried plums each day. Also called prunes, these fruits are shown to relieve constipation.4
Specific chronic constipation treatments – Fiber supplements
Fiber is a type of carbohydrate that can help increase bowel movements. Your healthcare provider might recommend taking a fiber supplement, such as a drink, or eating high fiber foods such as wheat bran or rye bread.3 Increase the fiber in your diet gradually to avoid gas or bloating.
Specific chronic constipation treatments – Laxatives
Laxatives are medications that help you have bowel movements. Some work with the water in your body, and some stimulate the nerves in your digestive system.
Laxatives called polyethylene glycol, lactulose, and bisacodyl are shown to help chronic constipation.3
Polyethylene glycol (PEG) and lactulose work with the water in your body to make bowel movements easier to pass, while bisacodyl stimulates your digestive system to get your bowels moving.
Specific chronic constipation treatments – Prosecretory agents
Other drugs, including linaclotide, lubiprostone, and plecanatide, can help chronic constipation. Each is taken as a daily pill. These medicines help your body release water into the digestive system, helping to relieve constipation.
Specific chronic constipation treatments – 5-HT4 receptor agonists
Medicines called 5-HT4 receptor agonists help the digestive system work more effectively to relieve constipation. One of them, prucalopride, is available in the United States and others are being studied in clinical trials.6
Specific chronic constipation treatments – Bile acid transporter inhibitors
A new medicine called elobixibat keeps digestive acids flowing in the lower intestine and helps this area stay more active, helping to relieve constipation. Elobixibat is approved in Japan and other countries in Asia, but not yet available elsewhere.7
Specific chronic constipation treatments – Probiotics
Supplements called probiotics add good bacteria to your digestive system. They can help some digestive problems, but it is important to always discuss use of probiotics with your physician before taking them. But so far, research does not show that they help with chronic constipation.3
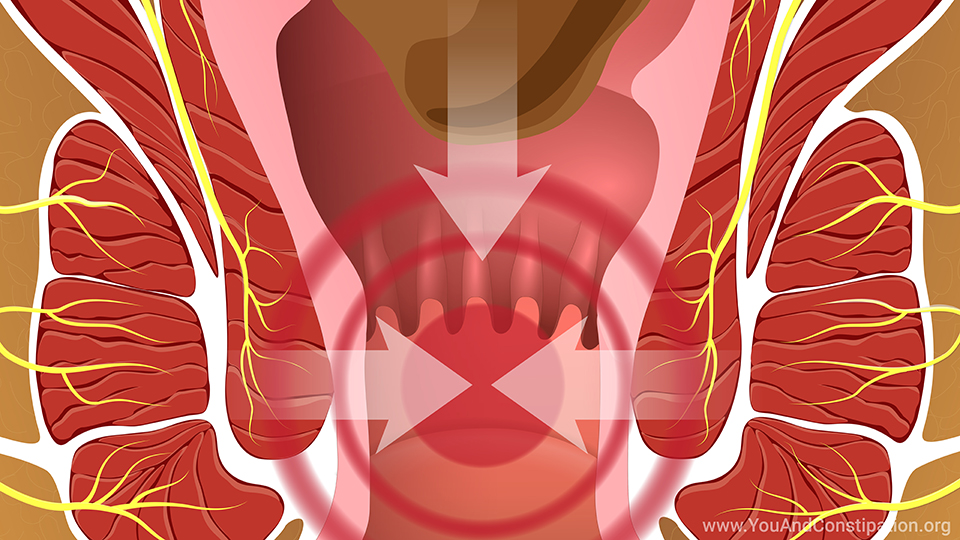
Specific chronic constipation treatments – Biofeedback training
At times, the muscles of the rectum and anus do not work well together. This can cause constipation by making it difficult for bowel movements to leave the body.
If this is the source of your chronic constipation, you might work with a physical therapist or nurse, using a technique called biofeedback training. It helps you train your body to push with one group of muscles while relaxing the other.3
The standard of care for managing and treating chronic constipation
If you have chronic constipation, the recommended treatments include adjusting your diet, fiber intake, and exercise level. If those do not relieve constipation, your physician is likely to recommend laxatives, and other medicines if laxatives do not work.
You may also have tests to check how your muscles are working when you have bowel movements, and you might work with a physical therapist.7
New treatments for chronic constipation – Clinical trials
Finally, you might want to join a research study for new treatments. Visit www.iffgd.org and select "Take Part in a Research Study" to find studies on chronic constipation. Or ask your physician where to find research studies.
Questions for your physician
Other questions to ask your physician are how they know you have chronic constipation and what diet and lifestyle changes they recommend. You may want to ask if you should try a laxative now or wait until after trying diet, exercise, and other changes.
If treatment has not worked so far, you might ask which medications they think may work best for you. Talking with your physician and asking questions is the best way to get treatment that helps your chronic constipation.
References
- Simren M, Palsson OS, Whitehead WE. Update on Rome IV Criteria for Colorectal Disorders: Implications for Clinical Practice. Curr Gastroenterol Rep 2017;19(4):15. doi:10.1007/s11894-017-0554-0
- About constipation. International Foundation for Gastrointestinal Disorders. Available at https://www.aboutconstipation.org/. Accessed December 2019.
- Ford AC, Moayyedi P, Lacy BE, et al. American College of Gastroenterology monograph on the management of irritable bowel syndrome and chronic idiopathic constipation. Am J Gastroenterol 2014;109(S1):S2-S26.
- Attaluri A1, Donahoe R, Valestin J, Brown K, Rao SS. Randomised clinical trial: dried plums (prunes) vs. psyllium for constipation. Aliment Pharmacol Ther 2011 Apr;33(7):822-8. doi: 10.1111/j.1365-2036.2011.04594.x. Epub 2011 Feb 15.
- Jiang C, Xu Q, Wen X, Sun H. Current developments in pharmacological therapeutics for chronic constipation. Acta Pharm Sin B 2015;5(4):300-309. doi:10.1016/j.apsb.2015.05.006
- Abireo Pharmaceuticals, Inc. Elobixibat. Available at https://www.albireopharma.com/programs/elobixibat. Accessed December 2019.
- Tse Y, Armstrong D, Andrews CN, et al. Treatment algorithm for chronic idiopathic constipation and constipation-predominant irritable bowel syndrome derived from a Canadian national survey and needs assessment on choices of therapeutic agents. Can J Gastroenterol Hepatol 2017;2017:8612189.
- International Foundation for Gastrointestinal Disorders. Industry Treatment News. Available at https://www.iffgd.org/2016-02-03-16-23-00.html. Accessed December 2019.
- Simren M, Palsson OS, Whitehead WE. Update on Rome IV criteria for colorectal disorders: implications for clinical practice. Curr Gastroenterol Rep 2017;19(4):15. doi:10.1007/s11894-017-0554-0
- Lacy BE, Mearin F, Chang L, et al. Bowel disorders. Gastroenterology 2016;150(6):1393-1407.
- Black CJ, Ford AC. Chronic idiopathic constipation in adults: epidemiology, pathophysiology, diagnosis and clinical management. Med J Aust 2018;209(2):86-91.
- Andrews CN, Storr M. The pathophysiology of chronic constipation. Can J Gastroenterol 2011;25(SB):16B-21B.
- Rao SS, Benninga M, Bharucha A, Chiarioni G, Di Lorenzo C, Whitehead W. ANMS-ESMN – Position paper and Consensus Guidelines on Biofeedback Therapy for Anorectal Disorders. Neurogastroenterol Motil 2015;27(5):594-609.
- Yan Y, Jimenez E, Sharma A, Eubanks A, Karunaratne T, Herekar A, Sanku A, Rao S. Evaluation and Validation of Mobile Phone APP for Assessment of Bowel Function in Healthy Subjects. Neurogastroenterology Motility 2020 March.
This slide show provides an overview of what you can do to manage and treat
chronic constipation (
CC), including exercise, dietary changes, and medications. It describes fiber supplements, laxatives, and medications such as prosecretory agents, 5-HT
4 receptor agonists, bile acid transporter inhibitors, probiotics, biofeedback training, and how to enroll in clinical trials.
-
Share with family and friends:
Click here to take our SURVEY
Your feedback is important to us! We will use your feedback to develop future areas of content about constipation which will help other patients, caregivers and families.