Managing and Treating IBS with Constipation
*Please note: This slide show represents a visual interpretation and is not intended to provide, nor substitute as medical and/or clinical advice.
What is IBS-C?
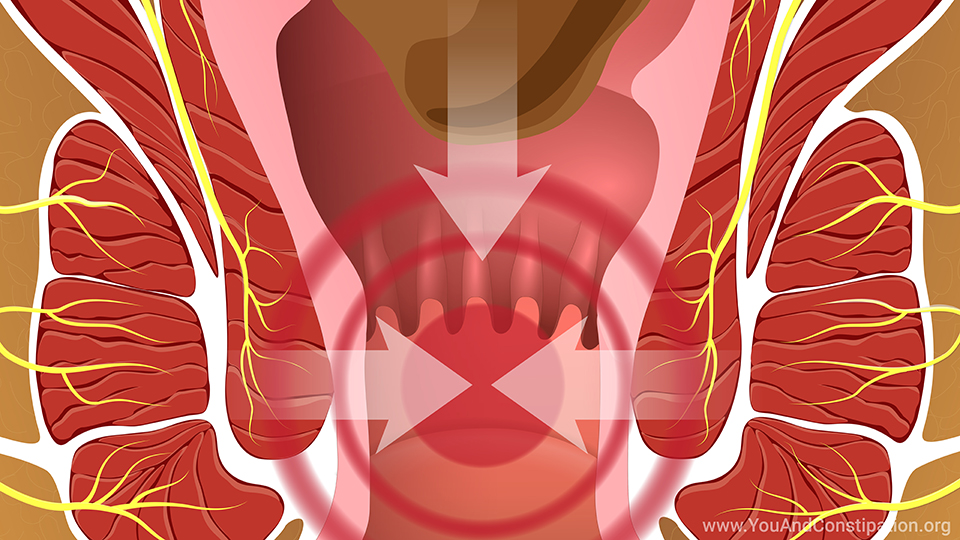
Irritable bowel syndrome with constipation, (IBS-C), is a condition that causes abdominal pain or discomfort along with changes in bowel movements.
Your bowel movements might be small, hard, and less frequent than usual. Some physicians consider you to have constipation when you have fewer than 3 bowel movements a week.1 They might be difficult or painful to pass, and you might also have gas and feel bloated much of the time.
Managing IBS-C
This animation tells you what you can do to manage your IBS-C, including possible changes in your diet, fiber intake, and coping strategies for life events. It also gives you information on the main treatments that researchers have found are effective for IBS-C.
Diet and IBS-C
Eating can trigger IBS-C symptoms such as abdominal pain or discomfort. So many people with IBS believe they are sensitive to certain foods. However, it is important to check with your physician before avoiding specific foods or types of foods. Limiting your diet too much can keep you from getting the nutrition you need.2
Getting help with your diet
Talk to your physician about any diet changes. You may also want to find a dietitian who specializes in IBS and other digestive system disorders. One place to search for a dietitian is the International Foundation for Gastrointestinal Disorders website at www.iffgd.org.
The right type of fiber for IBS-C
Eating more fiber can help some kinds of constipation. With IBS-C, it is important to get the right type of fiber. For example, bran is popular, but does not break down in your digestive system. So, it can make bloating and abdominal pain or discomfort worse. A fiber called psyllium does break down and may help.2
A fruit-based fiber supplement consisting of prunes, pomegranate, blueberries and acai berries can also be helpful.
Over-the-counter laxatives for IBS-C
A laxative such as polyethylene glycol can make bowel movements larger and easier to pass. It does this by keeping more water in your digestive system. Polyethylene glycol is sold under several brand names in the United States. It may not relieve all IBS-C symptoms, but you may have bowel movements more often.3
Stress management
Anxiety and stress can play a role in IBS-C. Talking to a counselor, especially someone who knows about IBS, can help. Hypnosis can also help some people with IBS-C.2
Antispasmodic medicines
Medicines called "antispasmodics" relax the muscles in your digestive system to relieve cramping. These medicines have been used for years and many different ones are available. Talk with your physician about the best option.2
Peppermint oil
Taking specially coated peppermint oil helped some people in research studies and may help you. However, all studies did not use the same form of peppermint oil. Talk with your physician about the best form and dose of peppermint oil to take.1
Antidepressants
Antidepressant medicines, including selective serotonin reuptake inhibitors and tricyclic antidepressants, can help relieve IBS symptoms.4
Linaclotide, plecanatide and lubiprostone
There are three prescription drugs approved in the US to help IBS-C.2
Linaclotide and plecanatide can relieve pain and other symptoms of constipation and help you have more frequent bowel movements with softer consistency.
Lubiprostone can also help you have more frequent bowel movements but does not help with pain.
All these medications work by increasing the fluid secreted into your intestines. This relieves constipation symptoms.
5-HT4 medicines
Some medicines that act directly on the digestive system are used for other types of constipation, but also help IBS-C. For example, prucalopride is approved to treat constipation that is not related to IBS, but your physician may ask you to try it for IBS-C.3
Probiotics put healthy bacteria into your system in pills, drinks or sometimes foods. Some may help with gas and bloating in IBS-C. But no one type is right for everyone.2 Ask your physician about which probiotics to take if you are interested. Natural probiotics such as yogurt might also help.
Antibiotics are not usually prescribed for IBS-C. You may ask your physician about them, but it is very important not to overuse these medicines. So you will probably take other medicines for IBS-C.5
Clinical trials and how to enroll
Finally, you might want to join a research study for new IBS-C treatments. Visit www.iffgd.org and select "Take Part in a Research Study" to find studies on irritable bowel syndrome. Or ask your physician where to find research studies.
Usual care for managing and treating IBS-C
There is no single treatment that works for everyone with IBS-C. You might take medicines to relieve some symptoms and make lifestyle changes to help with others. You might also benefit most from a combination of treatments to relieve the different symptoms of IBS-C.
Questions to ask about IBS-C treatment
Ask your physician about any possible side effects of treatment. Also ask how to take any medication, such as with or without food or what time of day. Keeping in close touch with your physician is one of the best ways to manage your IBS symptoms.
References
- Simren M, Palsson OS, Whitehead WE. Update on Rome IV Criteria for Colorectal Disorders: Implications for Clinical Practice. Curr Gastroenterol Rep 2017;19(4):15. doi:10.1007/s11894-017-0554-0
- Ford AC, Moayyedi P, Lacy BE, et al. American College of Gastroenterology monograph on the management of irritable bowel syndrome and chronic idiopathic constipation. Am J Gastroenterol 2014;109(S1):S2-S26.
- Weinberg DS, Smalley W, Heidelbaugh JJ, Shahnaz S. American Gastroenterological Association Institute Guideline on the Pharmacological Management of Irritable Bowel Syndrome. Gastroenterology 2014;147:1146-1148.
- Drossman DA, Tack J, Ford AC, et al. Neuromodulators for functional gastrointestinal disorders (disorders of gut-brain interaction): A Rome Foundation working team report. Gastroenterology 2018;154:1140-1171.e1. doi: 10.1053/j.gastro.2017.11.279
- Pimentel M, Chang C, Chua KS, et al. Antibiotic treatment of constipation-predominant irritable bowel syndrome. Dig Disc Sci 2014;59:1278-1285. doi: 10.1007/s10620-014-3157-8. Epub 2014 May 1.
This slide show provides an overview of what you can do to manage and treat
irritable bowel syndrome with constipation (
IBS-C), including possible changes in your diet, fiber intake, and changes to lifestyle. It also gives you information on fiber supplements, laxatives, antispasmodics, peppermint oil, prosecretory agents, 5-HT
4 medicines, probiotics, and how to enroll in clinical trials.
-
Share with family and friends:
Click here to take our SURVEY
Your feedback is important to us! We will use your feedback to develop future areas of content about constipation which will help other patients, caregivers and families.